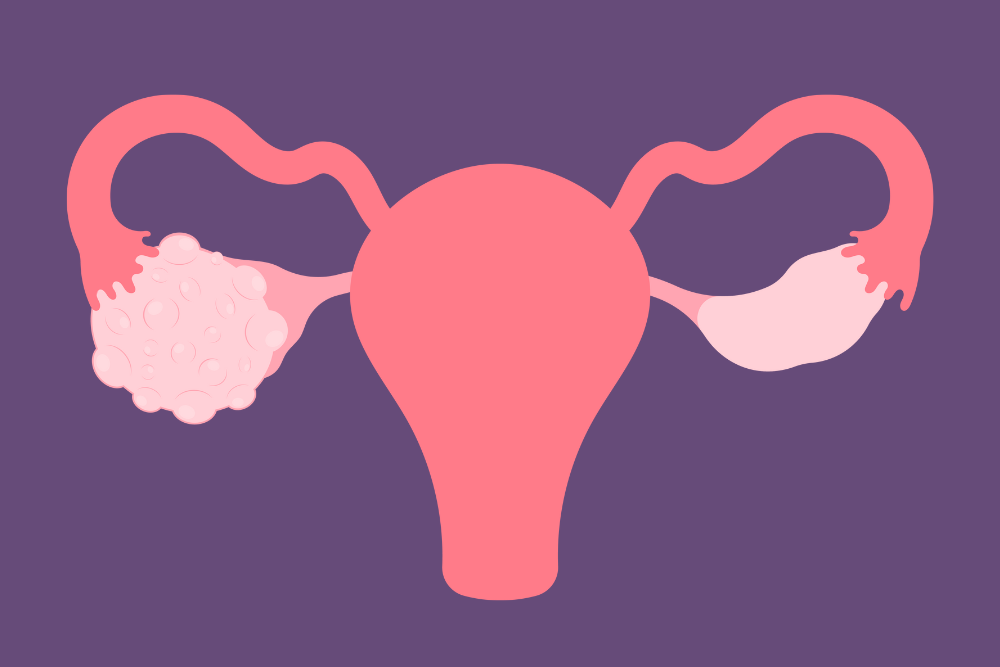
Traditional treatments for PCOS often focus on managing individual symptoms rather than addressing the root causes. This is where functional medicine comes into play, offering a holistic and integrative approach to PCOS treatment. PCOS functional medicine seeks to understand and treat the underlying imbalances in the body’s systems. In this blog, we will explore how a functional medicine approach can empower women with PCOS. Also, we will delve into the root cause and examples of PCOS functional medicine strategies.
Contents
Can Functional Medicine Help PCOS?
 Absolutely, functional medicine can be a valuable approach to managing Polycystic Ovary Syndrome (PCOS). Unlike conventional treatments, functional medicine seeks to identify and address the root causes of PCOS. This approach is holistic, considering a wide range of factors including hormonal imbalances, genetics, lifestyle, and environmental influences. In PCOS, issues such as insulin resistance, inflammation, and hormonal imbalances are common.
Absolutely, functional medicine can be a valuable approach to managing Polycystic Ovary Syndrome (PCOS). Unlike conventional treatments, functional medicine seeks to identify and address the root causes of PCOS. This approach is holistic, considering a wide range of factors including hormonal imbalances, genetics, lifestyle, and environmental influences. In PCOS, issues such as insulin resistance, inflammation, and hormonal imbalances are common.
Thus, PCOS functional medicine practitioners use comprehensive assessments to understand these underlying issues in each individual. They may employ advanced diagnostic testing to get a clearer picture of hormonal levels, insulin sensitivity, and other relevant markers. This detailed understanding allows for a more targeted and personalized treatment plan. This can lead to more effective management of the condition and an improvement in overall health and well-being.
What Is The Root Cause Of PCOS Functional Medicine?
This holistic approach considers multiple aspects of health and lifestyle to understand the unique manifestation of PCOS in each individual. Key factors that are often identified as root causes or significant contributors to PCOS in functional medicine include:
- Insulin Resistance: A primary factor in many cases of PCOS. Insulin resistance leads to higher insulin levels, which can stimulate the ovaries to produce more androgens (male hormones), contributing to PCOS symptoms like irregular periods, acne, and hair growth.
- Hormonal Imbalances: Besides insulin, imbalances in hormones such as estrogen, progesterone, and testosterone play a crucial role. High levels of androgens are a hallmark of PCOS, leading to many of the syndrome’s characteristic symptoms.
- Inflammation: Chronic low-grade inflammation has been linked to PCOS. This inflammation may stem from various sources, including dietary factors, lifestyle, stress, or environmental toxins, and can exacerbate hormonal imbalances and insulin resistance.
- Gut Health: Emerging research suggests a link between gut health and PCOS. Dysbiosis (imbalance in gut bacteria) and gut permeability can contribute to systemic inflammation and hormonal dysregulation.
- Genetic Predisposition: While not a direct cause, genetics can play a role in an individual’s susceptibility to PCOS. Those with a family history of PCOS are at a higher risk.
- Environmental Factors: Exposure to certain environmental toxins can disrupt endocrine function. These endocrine-disrupting chemicals can mimic, block, or interfere with hormones, potentially contributing to the development of PCOS.
Functional medicine aims to address these root causes through a personalized approach that includes dietary modifications, lifestyle changes, targeted supplementation, and possibly medication. The goal is to restore balance to the body’s systems, thereby alleviating the symptoms of PCOS and improving overall health.
What Are The Functional Medicines Tests For PCOS?
 Functional medicine employs a variety of tests to comprehensively evaluate and understand the underlying causes of Polycystic Ovary Syndrome (PCOS). These tests go beyond standard diagnostic criteria, focusing on a holistic view of health. Here are some key functional medicine tests used for PCOS:
Functional medicine employs a variety of tests to comprehensively evaluate and understand the underlying causes of Polycystic Ovary Syndrome (PCOS). These tests go beyond standard diagnostic criteria, focusing on a holistic view of health. Here are some key functional medicine tests used for PCOS:
Hormonal Testing
- Androgen Levels: Testing for elevated levels of male hormones, such as testosterone and DHEA-S, which are common in PCOS.
- Sex Hormone Binding Globulin (SHBG): Low levels of SHBG can be indicative of PCOS, as it affects the availability of testosterone in the body.
- Follicle Stimulating Hormone (FSH) and Luteinizing Hormone (LH): An altered LH to FSH ratio is often seen in PCOS.
- Prolactin: Elevated levels can mimic or exacerbate PCOS symptoms.
Insulin Resistance and Glucose Tolerance Tests
- Fasting Insulin and Glucose Levels: To assess insulin sensitivity.
- HOMA-IR: A calculation using fasting insulin and glucose levels to estimate insulin resistance.
- Oral Glucose Tolerance Test (OGTT): To evaluate how efficiently the body processes sugar, which is crucial in PCOS management.
Inflammatory Markers
- C-Reactive Protein (CRP): High levels can indicate inflammation in the body, which is linked to PCOS.
- Erythrocyte Sedimentation Rate (ESR): Another marker that can be used to assess inflammation.
Nutritional and Metabolic Panels
- Vitamin and Mineral Levels: Deficiencies in certain vitamins and minerals, such as Vitamin D, B vitamins, and magnesium, can exacerbate PCOS symptoms.
- Lipid Profile: Assessing cholesterol and triglycerides, as women with PCOS may have a higher risk of cardiovascular issues.
- Liver Function Tests: To assess liver health, which can be impacted by metabolic disturbances associated with PCOS.
Gut Health Assessments
- Comprehensive Stool Analysis: To evaluate gut microbiome balance, digestion, absorption, and gut inflammation.
- Food Sensitivity Testing: Identifying potential food sensitivities or intolerances that can contribute to systemic inflammation and hormonal imbalances.
Adrenal Function Tests
- Cortisol Levels: Chronic stress can affect cortisol levels, which in turn can impact PCOS symptoms.
- DHEA-S: An adrenal hormone that can be elevated in PCOS and contribute to symptoms.
Thyroid Function Tests
- TSH, Free T3, Free T4, Reverse T3, and Thyroid Antibodies: Comprehensive thyroid testing is important as thyroid disorders can mimic or worsen PCOS symptoms.
These tests provide a detailed picture of a woman’s hormonal balance, nutritional status, gut health, and more. This comprehensive information allows for a more targeted and effective approach to treating PCOS in the context of functional medicine.
What Are The Examples of PCOS Functional Medicine?
 Functional medicine offers a comprehensive and personalized approach to managing Polycystic Ovary Syndrome (PCOS). Here are some examples of how functional medicine might address PCOS:
Functional medicine offers a comprehensive and personalized approach to managing Polycystic Ovary Syndrome (PCOS). Here are some examples of how functional medicine might address PCOS:
Dietary Changes
Nutrition plays a critical role in managing PCOS. A low glycemic index diet. This includes foods that slowly release glucose into the bloodstream, which can be particularly beneficial for women with PCOS. This approach helps in managing insulin resistance, a common issue in PCOS. Emphasizing a diet rich in anti-inflammatory foods, such as those high in omega-3 fatty acids, antioxidants, and fiber, can also help combat the chronic inflammation often associated with PCOS.
Lifestyle Modifications
Incorporating regular physical activity is key in managing PCOS. A combination of cardiovascular exercise and strength training can improve insulin sensitivity, promote weight loss, and reduce the risk of cardiovascular disease. Stress management is equally important. Chronic stress can exacerbate PCOS symptoms by disrupting hormonal balance. Practices like yoga, meditation, and mindfulness can be effective in reducing stress levels.
Supplements and Herbal Remedies
Inositol, particularly myo-inositol, is a supplement that has shown promise in improving insulin sensitivity and promoting ovulation in women with PCOS. Omega-3 fatty acids can help reduce inflammation and improve hormonal balance. Spearmint tea has been studied for its potential to reduce androgen levels, which are typically high in PCOS. Additionally, vitamin D and magnesium supplements are often recommended, as deficiencies in these nutrients are common in PCOS and can impact insulin and hormonal balance.
Gut Health Improvement
A healthy gut microbiome is essential for overall health and can influence inflammation and hormonal balance. Probiotics and prebiotics can support gut health. Elimination diets can be useful in identifying and removing food sensitivities that might be contributing to gut issues and systemic inflammation, which in turn can affect PCOS symptoms.
Hormonal Therapies
Some women with PCOS may benefit from natural progesterone to help balance hormones and regulate menstrual cycles. Metformin, a medication more commonly used in conventional treatments, is sometimes utilized in functional medicine to improve insulin sensitivity, particularly in women who struggle with weight management or who are pre-diabetic.
Detoxification Support
Reducing exposure to endocrine disruptors, found in some plastics, pesticides, and personal care products, is important in managing PCOS. Supporting liver health through diet and supplements can enhance the body’s natural detoxification processes, helping to balance hormones and improve PCOS symptoms.
Comprehensive Testing
Detailed hormone testing can provide insights into specific hormonal imbalances that need to be addressed. Insulin resistance markers, such as fasting insulin and glucose levels and HOMA-IR, are critical in understanding and managing PCOS. Inflammatory markers like C-reactive protein (CRP) can also provide valuable information about the level of systemic inflammation.
Mind-Body Approaches
Techniques like acupuncture have been explored for their potential benefits in balancing hormones and improving menstrual regularity in women with PCOS. Cognitive Behavioral Therapy (CBT) can be effective in addressing mental health issues like anxiety or depression that often accompany PCOS, helping to improve overall quality of life.
Each of these approaches emphasizes the importance of a personalized treatment plan in functional medicine. And, recognizing that each individual with PCOS may have different underlying causes and therefore may respond differently to various treatments.
Conclusion
In conclusion, PCOS functional medicine offers a comprehensive and personalized approach, addressing the condition from various angles. By focusing on dietary changes, lifestyle modifications, specific supplements, and a deep understanding of individual hormonal and metabolic profiles, functional medicine aims to tackle the root causes of PCOS. This approach goes beyond just treating symptoms, emphasizing overall health and wellness.
The use of targeted functional medicine tests helps in creating a tailored treatment plan that can lead to significant improvements. Ultimately, this holistic strategy empowers women to regain control over their health and well-being. If you are facing PCOS-related issues, PCOS treatment at HerMantra can help. Book your free trial online pcos treatment session now.