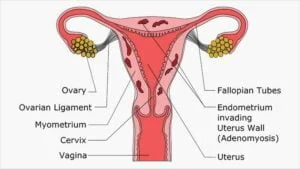
Entering menopause is a significant phase in a woman’s life, marked by various physical and hormonal changes. For those who have been grappling with endometriosis, a condition where tissue similar to the lining of the uterus grows outside the womb, the transition to menopause can bring both relief and new challenges. In this blog, we will explore the complexities of managing endometriosis during menopause, shedding light on effective endometriosis menopause treatment options, lifestyle adjustments, and the crucial support systems available.
Contents
What Is Endometriosis In Menopause?
 Endometriosis through menopause represents a complex journey for individuals facing the coalescence of these two distinct phases in a woman’s reproductive life. Menopause, marked by the cessation of menstrual cycles, typically brings relief from endometriosis symptoms for many women. However, the experience varies, with some individuals witnessing a reprieve, while others encounter persistent challenges.
Endometriosis through menopause represents a complex journey for individuals facing the coalescence of these two distinct phases in a woman’s reproductive life. Menopause, marked by the cessation of menstrual cycles, typically brings relief from endometriosis symptoms for many women. However, the experience varies, with some individuals witnessing a reprieve, while others encounter persistent challenges.
Hormonal fluctuations during menopause can influence the behavior of endometriotic lesions, potentially impacting symptom severity. Understanding the nuances of managing endometriosis through menopause requires a multifaceted approach, encompassing medical interventions, holistic wellness strategies, and emotional well-being considerations. This journey underscores the importance of personalized care, empowerment, and a supportive community.
What Is The Natural Endometriosis Menopause Treatment?
Natural endometriosis menopause treatment focuses on holistic approaches to manage symptoms and support overall well-being during the transition into menopause. While individual experiences vary, and consulting with a healthcare professional is essential, here are some natural strategies that some individuals find beneficial:
Dietary Modifications
Adopting an anti-inflammatory diet can be a cornerstone in managing endometriosis symptoms during menopause. Emphasizing a plant-based approach with ample fruits, vegetables, and whole grains while minimizing processed foods, red meat, and dairy may help alleviate inflammation associated with endometriosis. Additionally, incorporating omega-3 fatty acids from sources like flaxseeds, chia seeds, and fatty fish can contribute to an anti-inflammatory effect.
Herbal Supplements
Some individuals explore the potential benefits of herbal supplements in managing endometriosis symptoms during menopause. Turmeric, known for its anti-inflammatory properties, ginger, and chasteberry (Vitex), thought to regulate hormonal balance, are among the herbs considered. However, it’s crucial to approach these supplements with caution and consult with a healthcare provider, as they may interact with other medications or have varying effects on different individuals.
Mind-Body Practices
Stress management is paramount in addressing endometriosis symptoms. Mind-body practices such as yoga, meditation, and deep breathing exercises offer not only relaxation but also potential relief from pain and discomfort. These practices promote overall mental well-being and resilience during the menopausal transition.
Acupuncture
Traditional Chinese medicine, including acupuncture, is recognized by some individuals as a complementary therapy for managing pain associated with endometriosis. Acupuncture involves the insertion of thin needles into specific points on the body, aiming to stimulate energy flow and alleviate discomfort. While research on its efficacy is ongoing, some women find it beneficial in managing symptoms.
Regular Exercise
Engaging in regular physical activity is vital for managing both stress and endometriosis symptoms. Exercise helps regulate hormones, maintain a healthy weight, and alleviate pelvic pain. Low-impact activities like walking, swimming, or cycling can be particularly beneficial for women experiencing discomfort.
Adequate Sleep
Prioritizing good sleep hygiene is essential for overall well-being. Quality sleep contributes to hormonal balance and immune function, potentially influencing the severity of endometriosis symptoms. Establishing a consistent sleep routine, creating a comfortable sleep environment, and managing stress can enhance the quality of sleep during menopause.
Maintaining a Healthy Weight
Striving for and maintaining a healthy weight is crucial for managing endometriosis symptoms. Excess body weight can contribute to inflammation and hormonal imbalances, exacerbating symptoms. A balanced diet, coupled with regular exercise, supports weight management and overall health, potentially alleviating the impact of endometriosis during menopause.
While these natural approaches offer potential benefits, individuals must consult with their healthcare providers before making significant changes to their lifestyle or incorporating supplements, ensuring that these strategies align with their overall health and medical history. Personalized guidance is key in navigating natural endometriosis menopause treatments effectively.
When Should I Seek Medical Attention For Endometriosis Menopause?
 If you are experiencing endometriosis symptoms during menopause, it’s essential to stay vigilant about your health and seek medical attention if you encounter any of the following scenarios:
If you are experiencing endometriosis symptoms during menopause, it’s essential to stay vigilant about your health and seek medical attention if you encounter any of the following scenarios:
- New or Worsening Symptoms: If you notice new or worsening symptoms associated with endometriosis, such as pelvic pain, abdominal discomfort, or changes in bowel or bladder habits, it’s crucial to consult with your healthcare provider. Any abrupt changes in the pattern or severity of symptoms should be addressed promptly.
- Unexplained Pelvic Pain: Persistent or severe pelvic pain that cannot be attributed to other causes requires medical evaluation. Endometriosis-related pain during menopause should not be ignored, as it may indicate underlying issues that need attention.
- Irregular Bleeding or Spotting: Menopause typically involves the cessation of menstrual cycles. If you experience irregular bleeding or spotting, it may be a cause for concern and warrants a medical evaluation. This could be related to hormonal fluctuations or, in some cases, other gynecological issues.
- Difficulty Coping Emotionally: Menopause, coupled with the challenges of managing endometriosis, may impact your emotional well-being. If you find it challenging to cope emotionally, experiencing anxiety, depression, or mood swings, seeking mental health support is crucial. Your healthcare provider can help connect you with appropriate resources.
- Concerns About Fertility: If you have concerns about fertility during menopause or are contemplating assisted reproductive technologies, it’s important to discuss these matters with your healthcare provider. They can provide guidance on available options and potential implications.
Remember, proactive communication with your healthcare provider is key to managing endometriosis during menopause effectively. Regular check-ups, open discussions about your symptoms, and collaboration with your healthcare team will help ensure that you receive appropriate care tailored to your unique needs.
What Is The Best Treatment For Endometriosis Menopause?
The optimal treatment for endometriosis menopause varies depending on individual circumstances, symptoms, and the overall health of the person. It’s important to note that menopause itself can bring relief to many endometriosis symptoms due to the decline in estrogen levels. However, some women may still experience residual symptoms or complications.
Here are common endometriosis menopause treatment options:
Hormone Replacement Therapy (HRT)
For women undergoing menopause, hormone replacement therapy (HRT) is a common approach. This involves supplementing the body with estrogen or a combination of estrogen and progesterone to alleviate menopausal symptoms. While HRT can relieve symptoms like hot flashes and vaginal dryness, it may not be suitable for those with a history of endometriosis, as it can potentially stimulate the growth of endometrial tissue.
Surgical Interventions
In cases where endometriosis symptoms persist or are severe, surgical interventions may be considered. This could involve removing endometriotic lesions, scar tissue, or, in some cases, a hysterectomy (removal of the uterus) or oophorectomy (removal of ovaries). However, these surgeries are usually reserved for situations where other treatments have not been effective, and the decision is carefully weighed based on factors such as the woman’s age, health status, and desire for fertility preservation.
Pain Management
Chronic pain associated with endometriosis can be managed through pain medications, including nonsteroidal anti-inflammatory drugs (NSAIDs) or, in more severe cases, prescription pain medications.
Complementary Therapies
 Some individuals find relief from symptoms through complementary therapies such as acupuncture, physical therapy, or alternative medicine. While these approaches may provide relief for some, it’s essential to discuss their use with healthcare providers and ensure they complement conventional medical treatments.
Some individuals find relief from symptoms through complementary therapies such as acupuncture, physical therapy, or alternative medicine. While these approaches may provide relief for some, it’s essential to discuss their use with healthcare providers and ensure they complement conventional medical treatments.
The choice of treatment should be personalized, taking into account the severity of symptoms, individual health history, and future fertility desires. Consulting with a healthcare provider, preferably a specialist in reproductive health or gynecology, is crucial. They will help in developing an appropriate treatment plan.
Conclusion
In conclusion, navigating endometriosis through menopause demands a multifaceted and personalized approach that encompasses medical interventions, holistic wellness strategies, and a resilient mindset. As women transition into this transformative phase, the interplay between hormonal changes and endometriosis symptoms adds a layer of complexity. From exploring dietary modifications, and embracing mind-body practices to addressing emotional well-being and seeking community support, the journey requires an amalgamation of strategies.
By embracing this holistic approach and collaborating closely with healthcare providers, women can empower themselves to effectively manage the unique challenges. Ultimately, fostering a path to sustained well-being and resilience. If you are facing menopause related issues, menopause treatment at HerMantra can help. Book your free trial online menopause treatment session now.