In a world where women’s health is gaining increased attention and understanding, one condition stands out as both prevalent and enigmatic: Polycystic Ovary Syndrome (PCOS). This hormonal disorder affects millions of women worldwide, often presenting a myriad of symptoms that extend beyond reproductive health. Here, we will delve into its multifaceted PCOS causes, exploring the interplay of genetics, lifestyle factors, and hormonal imbalances.
Contents
What Are The Main PCOS Causes?
 Polycystic Ovary Syndrome (PCOS) is a complex hormonal disorder with a range of contributing factors. While the exact PCOS cause remains elusive, several key elements are known to play a role in the development and manifestation of PCOS. Here are the main PCOS causes:
Polycystic Ovary Syndrome (PCOS) is a complex hormonal disorder with a range of contributing factors. While the exact PCOS cause remains elusive, several key elements are known to play a role in the development and manifestation of PCOS. Here are the main PCOS causes:
Genetics
PCOS often exhibits a familial pattern, suggesting a genetic predisposition. Women with a family history of PCOS, especially with first-degree relatives like mothers or sisters affected, face an increased risk of developing the condition. While specific genes linked to PCOS have been identified, the complex interplay of multiple genetic factors makes it challenging to pinpoint a single causative gene. Genetic susceptibility may influence hormonal regulation and ovarian function, contributing to the manifestation of PCOS.
Insulin Resistance
Insulin resistance is a key player in PCOS development. When cells become less responsive to insulin, the body compensates by producing more insulin. Elevated insulin levels stimulate the ovaries to produce excess androgens, leading to hormonal imbalances. Insulin resistance is closely tied to obesity and lifestyle factors, making weight management and adopting a healthy diet crucial components in addressing PCOS.
Hormonal Imbalances
PCOS is characterized by disturbances in the normal hormonal regulation of the reproductive system. Elevated levels of luteinizing hormone (LH) and insulin, along with increased androgen production, contribute to irregular menstrual cycles, anovulation, and characteristic symptoms like acne and hirsutism. The intricate interplay between these hormones disrupts the delicate balance necessary for regular ovulation and menstrual cycles.
Inflammation
Chronic low-grade inflammation is increasingly recognized as a contributing factor in PCOS. Inflammation can adversely affect insulin sensitivity, exacerbating insulin resistance and hormonal imbalances. Adipose tissue, particularly in individuals with obesity, releases inflammatory cytokines that contribute to the inflammatory milieu associated with PCOS. Addressing inflammation through lifestyle changes and, in some cases, anti-inflammatory medications may play a role in managing PCOS symptoms.
High Androgen Levels
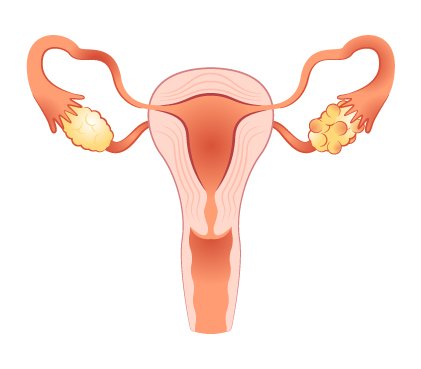
Elevated levels of androgens, such as testosterone, are a hallmark of PCOS and contribute to the characteristic symptoms experienced by affected individuals. Increased androgen levels are responsible for acne, hirsutism, and male-pattern hair loss. The ovaries in women with PCOS produce excess androgens, disrupting normal ovarian function and contributing to irregularities in the menstrual cycle. While androgens are naturally present in both men and women, an excess in women with PCOS can lead to the development of ovarian cysts and hinder regular ovulation.
Environmental Factors
 Emerging research suggests that exposure to environmental factors and endocrine-disrupting chemicals may influence the development of PCOS. These substances, found in certain pollutants, plastics, and pesticides, can interfere with hormonal balance and reproductive function. While the specific environmental triggers for PCOS are not fully elucidated, the potential impact of these factors underscores the importance of understanding the broader context in which PCOS may arise.
Emerging research suggests that exposure to environmental factors and endocrine-disrupting chemicals may influence the development of PCOS. These substances, found in certain pollutants, plastics, and pesticides, can interfere with hormonal balance and reproductive function. While the specific environmental triggers for PCOS are not fully elucidated, the potential impact of these factors underscores the importance of understanding the broader context in which PCOS may arise.
Irregular Fetal Development
Some researchers propose that irregularities in fetal development may contribute to the later development of PCOS. Exposure to elevated androgen levels during fetal development, either due to genetic factors or environmental influences, may influence the programming of the reproductive system. This early-life alteration could set the stage for the manifestation of PCOS during adolescence or adulthood.
Chronic Stress
Chronic stress has been implicated as a potential contributor to PCOS. The stress hormone cortisol, when consistently elevated, can impact the delicate balance of reproductive hormones. Stress-induced changes in the hypothalamus-pituitary-adrenal (HPA) axis may disrupt normal ovarian function and contribute to irregular menstrual cycles. Additionally, stress can exacerbate inflammation and insulin resistance, further complicating the hormonal milieu associated with PCOS.
Understanding the interplay of these factors is essential for managing and treating PCOS effectively. It’s important to note that the combination and severity of these causes can vary among individuals, contributing to the heterogeneity of PCOS presentations. Lifestyle modifications, medication, and targeted interventions can help address these underlying causes and alleviate symptoms associated with PCOS.
Can Lifestyle Cause PCOS?
Yes, lifestyle factors can play a significant role in the development and exacerbation of Polycystic Ovary Syndrome (PCOS). While genetics also contribute to PCOS, lifestyle choices can influence hormonal balance, insulin resistance, and overall reproductive health. Here are ways in which lifestyle factors can contribute to PCOS:
Obesity
Obesity is strongly associated with PCOS. Excess adipose tissue can contribute to insulin resistance, leading to elevated insulin levels. Insulin resistance, in turn, stimulates the ovaries to produce more androgens, contributing to hormonal imbalances characteristic of PCOS.
Dietary Habits
Poor dietary choices, especially diets high in refined carbohydrates and sugars, can contribute to insulin resistance. Diets that lead to rapid spikes in blood sugar levels may exacerbate hormonal imbalances associated with PCOS. A balanced diet that includes whole grains, fruits, vegetables, and lean proteins can help regulate blood sugar and improve insulin sensitivity.
Physical Activity
Sedentary lifestyles are linked to an increased risk of PCOS. Regular physical activity has been shown to improve insulin sensitivity and help with weight management. Exercise can also have direct benefits on reproductive health by promoting regular menstrual cycles and reducing symptoms of PCOS.
Sleep Patterns
Disrupted sleep patterns or insufficient sleep may contribute to hormonal dysregulation and insulin resistance. Adequate, quality sleep is crucial for overall health and hormonal balance. Establishing a regular sleep routine and addressing sleep disturbances can be beneficial for individuals with PCOS.
Smoking and Alcohol Consumption
Smoking and excessive alcohol consumption have been associated with an increased risk of PCOS. These lifestyle factors can disrupt hormonal balance and have negative effects on reproductive health. Quitting smoking and moderating alcohol intake may be advisable for individuals with PCOS.
While lifestyle factors can contribute to the development of PCOS, it’s important to note that these factors interact with genetic predispositions. Adopting a healthy lifestyle can be beneficial for managing PCOS symptoms and improving overall well-being. Consulting with healthcare professionals for personalized advice and treatment is crucial for individuals with PCOS.
What Are Some Warning Signs To Look For?
 Not every individual with PCOS will experience the same symptoms, and the severity of symptoms can vary. However, the following are some common warning signs that may prompt further investigation:
Not every individual with PCOS will experience the same symptoms, and the severity of symptoms can vary. However, the following are some common warning signs that may prompt further investigation:
- Irregular Menstrual Cycles: Menstrual irregularities, such as infrequent or absent periods, can be a common indicator of PCOS. Some individuals may also experience heavy or prolonged menstrual bleeding.
- Ovulatory Dysfunction: PCOS often leads to anovulation, where the ovaries do not release eggs regularly. This can result in difficulties conceiving and infertility.
- Hirsutism (Excessive Hair Growth): Increased androgen levels in PCOS can cause hirsutism, which is the growth of coarse, dark hair in areas where men typically grow hair, such as the face, chest, and back.
- Acne and Oily Skin: Elevated androgen levels may contribute to acne and oily skin, particularly along the jawline, chin, and upper neck.
- Hair Loss: Thinning of hair or male-pattern baldness can occur in individuals with PCOS due to the influence of androgens on the hair follicles.
- Weight Gain and Difficulty Losing Weight: Many women with PCOS may struggle with weight management. Insulin resistance, common in PCOS, can contribute to weight gain and make it challenging to lose weight.
- Skin Darkening: Acanthosis nigricans, a condition characterized by darkened, thickened skin in body creases and folds, may be associated with insulin resistance seen in PCOS.
- Fatigue: Hormonal imbalances and disrupted sleep patterns associated with PCOS can contribute to fatigue and low energy levels.
- Mood Changes: Some individuals with PCOS may experience mood swings, anxiety, or depression. Hormonal fluctuations and the impact of PCOS on mental health can contribute to these symptoms.
- Pelvic Pain: Pelvic pain or discomfort may occur, especially in the presence of ovarian cysts. However, not all individuals with PCOS develop cysts, and their presence does not always cause pain.
It’s important to remember that the presence of one or more of these signs does not necessarily confirm a diagnosis of PCOS. If you are experiencing any of these warning signs or suspect you may have PCOS, it is advisable to consult with a healthcare professional for a thorough evaluation and appropriate management.
Conclusion
In conclusion, Polycystic Ovary Syndrome (PCOS) is a complex hormonal disorder that affects many women worldwide. PCOS causes are multifaceted, involving genetic predispositions, insulin resistance, hormonal imbalances, and lifestyle factors. While each person’s experience with PCOS is unique, understanding the interplay of these factors is crucial for effective management. Lifestyle changes also play a significant role in alleviating symptoms.
Seeking guidance from healthcare professionals is essential for a thorough diagnosis and personalized treatment plan. With awareness, knowledge, and proactive measures, women with PCOS can empower themselves to navigate this condition and enhance their overall well-being.
If you are facing PCOS related issues, pcos treatment at HerMantra can help. Book your free trial online pcos treatment session now.