Living with Polycystic Ovary Syndrome (PCOS) can be challenging, impacting various aspects of a woman’s life. From irregular menstrual cycles to hormonal imbalances, PCOS requires careful management to enhance overall well-being. One crucial aspect of PCOS treatment is progestin therapy, a hormonal approach that aims to restore balance and alleviate symptoms. In this blog, we will delve into the intricacies of progestin therapy for PCOS, exploring its mechanisms, benefits, and considerations for those seeking hormonal harmony.
Contents
What Is Progestin Therapy?
 Progestin therapy involves administering synthetic forms of progesterone, known as progestins. It is to address hormonal imbalances in the body. Progesterone is a natural hormone produced by the ovaries during the menstrual cycle and plays a crucial role in regulating the menstrual cycle, supporting pregnancy, and maintaining hormonal balance.
Progestin therapy involves administering synthetic forms of progesterone, known as progestins. It is to address hormonal imbalances in the body. Progesterone is a natural hormone produced by the ovaries during the menstrual cycle and plays a crucial role in regulating the menstrual cycle, supporting pregnancy, and maintaining hormonal balance.
In the context of polycystic ovary syndrome (PCOS), a common endocrine disorder among women, progestin therapy is often employed to counteract the elevated levels of androgens (male hormones) and irregular menstrual cycles characteristic of the condition. By introducing exogenous progestins, healthcare providers aim to mimic the hormonal effects of natural progesterone. Ultimately, promoting regular menstrual cycles, reducing androgen levels, and addressing various symptoms associated with PCOS.
Therefore, progestin therapy is commonly utilized for managing PCOS. Also in various other medical contexts, such as hormone replacement therapy and contraception. Its application underscores the importance of hormonal balance in maintaining overall reproductive health and well-being.
Which Progestin Is Best For PCOS?
The choice of the best progestin for PCOS can vary based on individual health considerations and treatment goals. Different progestins have unique properties, and healthcare providers may tailor their recommendations to address specific symptoms and patient needs. Here are some commonly used progestins for PCOS:
- Drospirenone: Often used in combination with ethinyl estradiol in oral contraceptives, drospirenone has anti-androgenic properties, making it beneficial for managing symptoms like acne and hirsutism (excess hair growth).
- Norethindrone: This progestin is commonly used in oral contraceptives and progestin-only pills. It is considered a versatile option with a lower risk of androgenic side effects, making it suitable for some individuals with PCOS.
- Medroxyprogesterone acetate (MPA): This progestin is available in oral, injectable, and intrauterine forms. It is often used to induce regular menstrual cycles in women with PCOS and can be administered in various formulations based on individual preferences and treatment goals.
- Norgestimate: Found in some combined oral contraceptives, norgestimate is a third-generation progestin with a relatively lower androgenic effect. It may be prescribed to address hormonal imbalances associated with PCOS.
- Dienogest: This progestin is known for its anti-androgenic properties and is sometimes used to manage symptoms like acne and hirsutism in women with PCOS.
It’s important to note that the selection of the most appropriate progestin should be made by a healthcare professional based on an individual’s medical history, specific PCOS symptoms, and other health considerations. Regular communication with a healthcare provider is crucial for monitoring progress and adjusting treatment plans.
What Is The Process Of Progestin Therapy For PCOS?
 The process of progestin therapy for PCOS involves a careful evaluation by a healthcare professional and the development of an individualized treatment plan. Here is a general overview of the steps involved in progestin therapy for PCOS:
The process of progestin therapy for PCOS involves a careful evaluation by a healthcare professional and the development of an individualized treatment plan. Here is a general overview of the steps involved in progestin therapy for PCOS:
Diagnosis and Evaluation
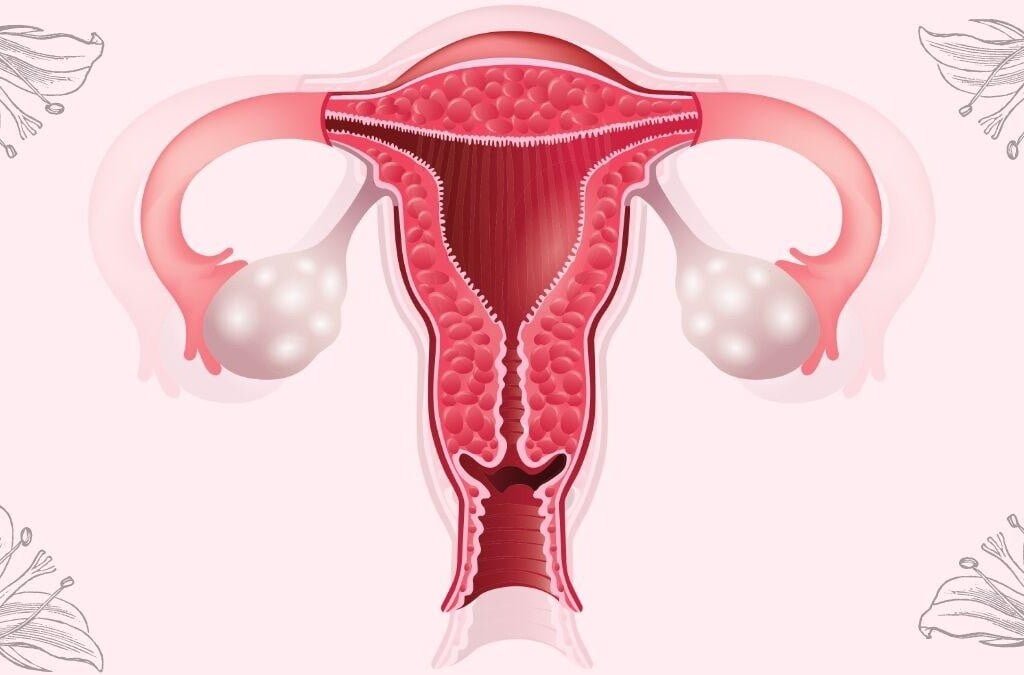
- In the diagnostic phase, healthcare providers consider symptoms like irregular menstrual cycles, elevated androgen levels, and the presence of ovarian cysts to diagnose PCOS.
- Blood tests are crucial for assessing hormonal levels, helping healthcare professionals understand the extent of hormonal imbalances.
- Ultrasound imaging provides a visual confirmation of polycystic ovaries and aids in evaluating the overall reproductive health.
Discussion of Treatment Goals
- Treatment goals are established through collaborative discussions between the healthcare provider and the individual with PCOS.
- Common goals include regulating menstrual cycles to promote regular ovulation, reducing elevated androgen levels, and addressing specific symptoms such as acne or hirsutism.
Prescription of Progestin
- Based on the identified treatment goals and the individual’s health profile, the healthcare provider prescribes an appropriate form of progestin.
- Oral contraceptives containing both estrogen and progestin or progestin-only pills are commonly prescribed. The choice depends on factors like the need for contraception and the presence of other health considerations.
Initiation of Treatment
- Clear instructions are provided on how to take the prescribed progestin, ensuring consistent and proper use.
- For oral contraceptives, individuals are typically advised to take a pill daily, preferably at the same time each day.
Monitoring and Adjustments
- Regular follow-up appointments are scheduled to monitor the individual’s response to progestin therapy.
- Blood tests may be conducted periodically to assess hormonal levels, helping healthcare providers make informed decisions about adjusting the treatment plan.
- Adjustments may involve changing the dosage or type of progestin to better suit the individual’s needs and minimize side effects.
Management of Side Effects
- Healthcare providers address any side effects experienced by individuals during progestin therapy.
- Common side effects may include nausea, breast tenderness, or mood changes. Adjustments to the treatment plan, such as changing the type of progestin or altering the dosage, can often alleviate these issues.
Lifestyle Modifications
- In conjunction with progestin therapy, healthcare providers may emphasize the importance of lifestyle modifications.
- Dietary changes and regular exercise can enhance the effectiveness of treatment, promoting overall health and well-being.
Long-Term Management
- Progestin therapy may be part of a comprehensive, long-term management plan for PCOS.
- For individuals seeking to regulate menstrual cycles or manage symptoms over an extended period, ongoing communication with healthcare providers and regular check-ups remain crucial.
Therefore, maintaining open communication with healthcare providers is essential for individuals. This can optimize the benefits of progestin therapy as part of their PCOS management strategy.
What Are The Benefits You Can Expect?
 Progestin therapy for PCOS can offer several benefits aimed at addressing hormonal imbalances and managing associated symptoms. Here are some potential benefits individuals may expect:
Progestin therapy for PCOS can offer several benefits aimed at addressing hormonal imbalances and managing associated symptoms. Here are some potential benefits individuals may expect:
- Regulation of Menstrual Cycles: Progestin therapy helps regulate menstrual cycles, promoting regular ovulation and reducing the frequency of irregular periods. This is a common challenge for women with PCOS.
- Reduction in Androgen Levels: Progestins, especially those with anti-androgenic properties, can help lower elevated levels of androgens (male hormones) commonly observed in individuals with PCOS. This may lead to improvements in symptoms such as acne and hirsutism (excess hair growth).
- Management of Ovulatory Dysfunction: For women with PCOS who experience anovulation (lack of ovulation), progestin therapy can induce regular ovulatory cycles, improving fertility and increasing the likelihood of conception.
- Support for Endometrial Health: Progestins help maintain a healthy endometrial lining by promoting regular shedding during menstruation. This can reduce the risk of endometrial hyperplasia, a condition associated with prolonged exposure to estrogen without sufficient progesterone.
- Improved Skin Health: Anti-androgenic progestins may have a positive impact on skin health, helping to reduce acne and oily skin associated with elevated androgen levels in PCOS.
- Enhanced Fertility: By promoting regular ovulation and addressing hormonal imbalances, progestin therapy can improve fertility in women with PCOS who are trying to conceive.
- Predictable Menstrual Cycles: Establishing regular menstrual cycles through progestin therapy can contribute to predictability, making it easier for individuals to plan and manage their daily lives.
Overall, it’s important to note that the benefits of progestin therapy can vary among individuals. So, the specific outcomes may depend on factors such as the type of progestin used, treatment duration, and individual response.
What Are Some Limitations Of Progestin Therapy For PCOS?
 While progestin therapy can be beneficial for managing certain aspects of polycystic ovary syndrome (PCOS), it also has some limitations and considerations. It’s essential to be aware of these factors when considering progestin therapy. Here are some limitations:
While progestin therapy can be beneficial for managing certain aspects of polycystic ovary syndrome (PCOS), it also has some limitations and considerations. It’s essential to be aware of these factors when considering progestin therapy. Here are some limitations:
- Variable Response
Individual responses to progestin therapy can vary. While some individuals may experience significant improvements in symptoms and hormonal balance, others may have a more limited response or may not tolerate certain progestins well.
- Temporary Relief
Progestin therapy provides symptomatic relief but does not cure PCOS. Its effects are often temporary, and discontinuation of treatment may result in a return of symptoms.
- Side Effects
Progestin therapy may be associated with side effects, including nausea, breast tenderness, mood changes, and irregular bleeding. The severity and occurrence of these side effects can vary among individuals.
- Masking Underlying Issues
While progestin therapy can regulate menstrual cycles, it may mask underlying issues such as insulin resistance, which is common in individuals with PCOS. Addressing the root causes of PCOS may require a more comprehensive approach.
- Impact on Bone Health
Prolonged use of progestins, particularly in high doses, may have implications for bone health. Healthcare providers need to monitor bone density and provide appropriate guidance on calcium and vitamin D intake.
- Contraindications
Certain medical conditions, such as a history of blood clots, liver disease, or certain types of cancer, may be contraindications for progestin therapy. Healthcare providers must carefully assess an individual’s health history before prescribing progestin.
- Impact on Mood and Libido
Some individuals may experience changes in mood or libido as a side effect of progestin therapy. It’s important to communicate openly with healthcare providers about such concerns.
Overall it’s crucial for individuals considering progestin therapy for PCOS to have open and ongoing communication with their healthcare providers. Hence, a comprehensive treatment plan may involve a combination of medications, lifestyle modifications, and other interventions.
Conclusion
In conclusion, exploring progestin therapy for PCOS reveals a multifaceted approach to managing this complex condition. From regulating menstrual cycles and reducing androgen levels to supporting fertility and alleviating symptoms, progestin therapy offers valuable benefits. However, it’s essential to acknowledge its limitations, including variable responses, temporary relief, and potential side effects.
Therefore, by understanding the role of progestin therapy, individuals with PCOS can make informed decisions. Thus, enhancing their overall well-being and navigating the challenges of this hormonal disorder. So, if you are facing PCOS-related issues, PCOS treatment at HerMantra can help. Book your free trial online pcos treatment session now.