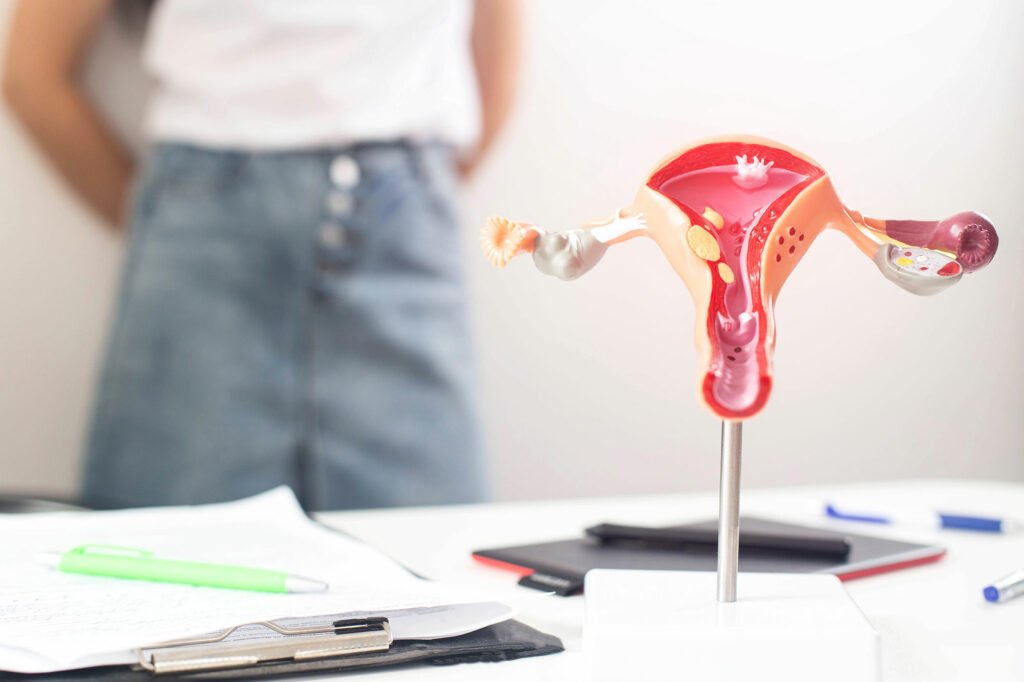
Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder affecting people with ovaries, often leading to fertility challenges. The impact of PCOS on fertility can be significant, but with advancements in medical science, there are various effective treatments available. In this comprehensive guide, we’ll explore PCOS and delve into the different PCOS fertility treatment that can help individuals with PCOS achieve their dream of parenthood.
Contents
What Does PCOS Fertility Mean?
PCOS fertility refers to the challenges and considerations related to fertility (the ability to conceive and have a successful pregnancy) in individuals who have been diagnosed with Polycystic Ovary Syndrome (PCOS). PCOS is a common hormonal disorder that affects people with ovaries and is often associated with reproductive and fertility issues. Understanding PCOS fertility involves recognizing how the condition can impact various aspects of the reproductive system and what measures can be taken to address these challenges.
Here are the key aspects of PCOS fertility:
- Irregular Ovulation: One of the primary concerns in PCOS fertility is irregular ovulation. Ovulation is the process where an egg is released from the ovary, and irregular ovulation can make it more difficult for individuals to conceive.
- Anovulation: In some cases, individuals with PCOS may experience anovulation, meaning they do not ovulate at all. This significantly reduces the chances of natural conception.
- Menstrual Irregularities: PCOS often causes irregular menstrual cycles. Menstrual irregularities can make it challenging to predict the fertile window, further complicating natural conception.
- Insulin Resistance: Insulin resistance, commonly associated with PCOS, can lead to difficulties in maintaining a healthy weight. Obesity and insulin resistance can negatively impact fertility and increase the risk of complications during pregnancy.
- Hormonal Imbalances: Elevated levels of androgens (male hormones) and imbalances in other reproductive hormones can affect the overall hormonal environment, making it harder for the reproductive system to function optimally.
- Increased Risk of Miscarriage: Individuals with PCOS may have a higher risk of miscarriage compared to those without the condition. This risk is influenced by factors such as insulin resistance and hormonal imbalances.
Addressing PCOS fertility often involves a combination of lifestyle modifications, medications, and, in some cases, assisted reproductive technologies.
PCOS Fertility Treatment Methods
Here are some common PCOS fertility treatment methods with detailed descriptions for each:
Lifestyle Changes

Ovulation Induction Medications
Ovulation induction medications are a common treatment approach for individuals experiencing difficulties with ovulation, a key factor in female fertility. These medications are designed to stimulate the ovaries to produce and release eggs, increasing the chances of conception. One widely used class of drugs for ovulation induction is selective estrogen receptor modulators (SERMs), such as clomiphene citrate.
Clomiphene citrate works by blocking estrogen receptors in the hypothalamus and pituitary gland, leading to an increase in the release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH). This hormonal boost stimulates the ovarian follicles, promoting the development and release of eggs.
Hormonal Therapy
Hormonal therapy, also known as hormone therapy, refers to the use of hormones or hormone-blocking agents to treat various medical conditions or manage hormonal imbalances in the body. This therapeutic approach is applied in diverse fields of medicine, including oncology, gynecology, endocrinology, and gender transition.
In the context of cancer treatment, hormonal therapy is often used to interfere with the growth of hormone-sensitive tumors. For example, in breast cancer, drugs like tamoxifen or aromatase inhibitors may be prescribed to block the effects of estrogen, a hormone that can stimulate the growth of certain types of breast cancer cells.
Similarly, in prostate cancer, hormonal therapies aim to reduce levels of testosterone or block its effects, as prostate cancer cells often depend on this hormone for growth.
Egg Freezing

Egg freezing, also known as oocyte cryopreservation, is a medical procedure that involves the extraction, freezing, and storage of a woman’s eggs (oocytes) for future use. This technology has become increasingly popular as a means for women to preserve their fertility, especially for those who may wish to delay childbearing due to career goals, educational pursuits, or other personal reasons.
The process typically begins with ovarian stimulation using hormones to encourage the ovaries to produce multiple eggs during a single menstrual cycle. This is monitored through blood tests and ultrasounds.
Once the eggs reach maturity, a minor surgical procedure known as egg retrieval is performed. During this outpatient procedure, a needle is guided through the vaginal wall to aspirate the eggs from the ovarian follicles.
Ovarian Drilling
Ovarian drilling is typically considered when other fertility treatments, such as medication (e.g., clomiphene citrate) and lifestyle changes, have not been successful.
During ovarian drilling, a surgeon uses a laparoscope (a thin, lighted tube with a camera) to access the ovaries through small incisions in the abdomen. Once the ovaries are visualized, the surgeon may use a laser or electrocautery to create a few punctures or “drill” tiny holes in the ovarian surface.
This procedure is thought to disrupt the ovarian tissue and reduce the production of androgens (male hormones) from the ovaries, helping to restore more normal ovulatory function.
Assisted Reproductive Technologies (ART)
Assisted Reproductive Technologies (ART) refer to a range of medical procedures that are used to treat infertility by manipulating eggs, sperm, or embryos outside the body. These technologies are employed when natural conception is not possible or has not been successful.
Several key ART methods include in vitro fertilization (IVF), intracytoplasmic sperm injection (ICSI), gamete intrafallopian transfer (GIFT), and zygote intrafallopian transfer (ZIFT), among others.
- In Vitro Fertilization (IVF): IVF is the most common and widely known form of ART. It involves stimulating the ovaries to produce multiple eggs, retrieving the eggs from the ovaries, fertilizing them with sperm in a laboratory dish, and then transferring the resulting embryos into the uterus. IVF is used for various infertility issues, including fallopian tube blockages, male factor infertility, and unexplained infertility.
- Intracytoplasmic Sperm Injection (ICSI): ICSI is a specialized form of IVF in which a single sperm is directly injected into an egg. This technique is particularly useful when there are severe male fertility issues, such as low sperm count or poor sperm motility.
How To Get PCOS Fertility Treatment?

Here are the steps you can take to pursue PCOS fertility treatment:
- Consult with a Healthcare Professional: Schedule an appointment with a healthcare provider, preferably a reproductive endocrinologist or fertility specialist. They can assess your medical history, perform necessary tests, and diagnose PCOS.
- Diagnostic Tests: Diagnostic tests may include blood tests to measure hormone levels (such as FSH, LH, and testosterone), imaging studies (ultrasound) to examine the ovaries, and other assessments to evaluate your reproductive health.
Conclusion
In conclusion, PCOS fertility presents a complex landscape of challenges and considerations for individuals with Polycystic Ovary Syndrome. The interplay of hormonal imbalances, irregular ovulation, and associated factors can significantly impact the ability to conceive and have a successful pregnancy. However, with advancements in medical science and a holistic approach to care, there are effective strategies to address PCOS-related fertility issues.
The evolving landscape of PCOS research and fertility treatments continues to offer new possibilities, providing optimism for those on the path to building a family despite the challenges posed by this common hormonal disorder.
If you are facing PCOS related issues, pcos treatment at HerMantra can help. Book your free trial online pcos treatment session now.